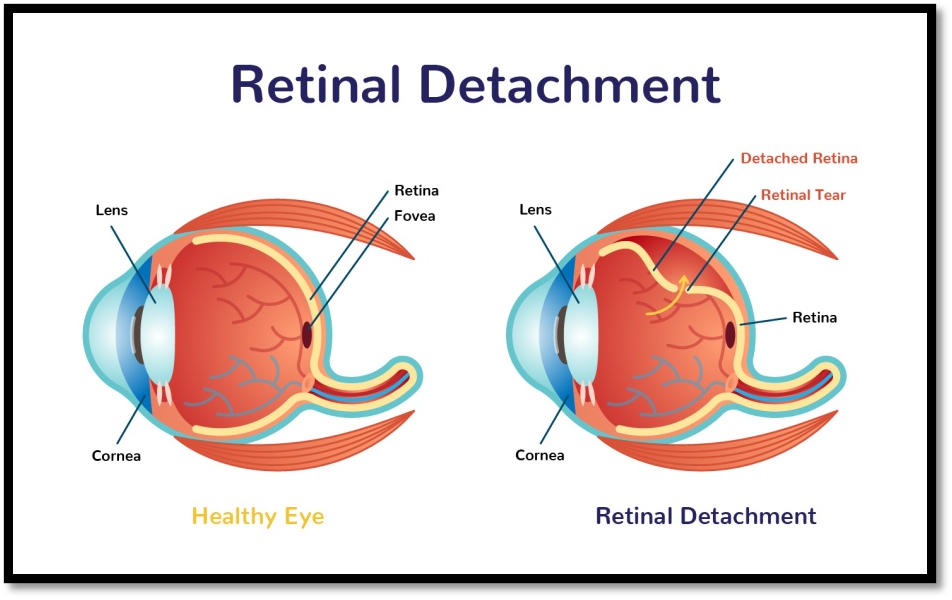
Your retina is the thin sensory membrane that lines the inner surface of the back of your eyeball. It consists of several layers of cells, one of which contains specialized cells called photoreceptors. The human eye is equipped with two types of photoreceptors: rods and cones.
When the retina becomes detached from the underlying supportive tissue, a condition called retinal detachment; it can put you at risk for serious sight loss. Retinal detachment can occur suddenly if the retina detaches immediately, but it can also occur slowly over time as the retina pulls away from the supportive tissue. This slowly progressing condition is called a retinal tear. A retinal tear, if left untreated, can progress to retinal detachment.
If your retina is not reattached quickly the damage may be permanent.
Symptoms to Consider
There are a variety of symptoms that individuals with retinal detachment or retinal tear may experience. These include:
- Loss of vision
- Spots in your vision
- Blurry vision
- Flashes
- Floaters
- A shadow or curtain descending over your vision, either from the top of your eye or from the side
There is no pain associated with retinal detachment or retinal tearing, but that does not mean that both conditions are not serious.
What Causes (or Potentially Causes) Retinal Detachment?
Trauma: A facial or eye injury can cause your retina to become detached. If you experience any trauma to your eyes or face you should monitor your vision carefully and look for signs of a retinal tear or retinal detachment.
Nearsightedness: Individuals who are extremely nearsighted are also at an increased risk for retinal detachment since their eyeballs are naturally quite long, which puts strain on the retina and the supportive tissue.
Eye Surgery: In some rare cases LASIK surgery or cataract surgery can inadvertently cause your retina to become detached, especially if you are already extremely nearsighted.
Diseases and Disorders: Eye diseases or tumors in your eye may also cause retinal detachment. Other conditions, such as diabetes and sickle cell disease, also put you at an increased risk for retinal detachment. Diabetic retinopathy, which causes new blood vessels to grow under your retina, may also push your retina away from the supportive tissue, causing retinal tearing or retinal detachment. Individuals with retinoschisis, uveitis, degenerative myopia, or lattice degeneration are also at an increased risk of retinal tearing or detachment.
Your Personal and Family History: Individuals who have a family history of retinal tearing or detachment may also be at an increased risk of retinal tearing or detachment. You are also more likely to be at risk for retinal tearing or detachment if your other eye has experienced either of these conditions.
Fluid movement within the eye can also, in rare cases, cause retinal detachment.
Who is Prone to Retinal Detachment?
According to the National Eye Institute individuals over the age of forty are more likely to experience retinal detachments or retinal tears. Men, as well as Caucasian individuals, are also more likely to experience retinal detachment then women or African Americans